When it comes to our health and well-being, there’s a fascinating and relatively new area of research known as the gut-brain connection. It examines the link between our digestive system, or “gut,” and our brain, and how these two seemingly separate entities communicate and influence each other.
Understanding the importance of this gut-brain connection is crucial as it has a profound impact on our overall health and wellness. In this section, we’ll explore the significance of the gut-brain connection and provide an overview of the intricate relationship between our gut and brain, known as the gut-brain axis.
| Key Takeaways |
|---|
| The Gut-Brain Connection is essential for overall health and wellness, facilitating two-way communication between the gut and the brain. |
| The Vagus Nerve is a crucial component in Gut-Brain Communication, transmitting signals between the gut and the brain, influencing bodily functions and emotions. |
| Neurotransmitters like serotonin and GABA in the Gut-Brain Connection play a significant role in regulating emotions and mental health, with their production in the gut impacting overall well-being. |
The Gut-Brain Connection and its Importance
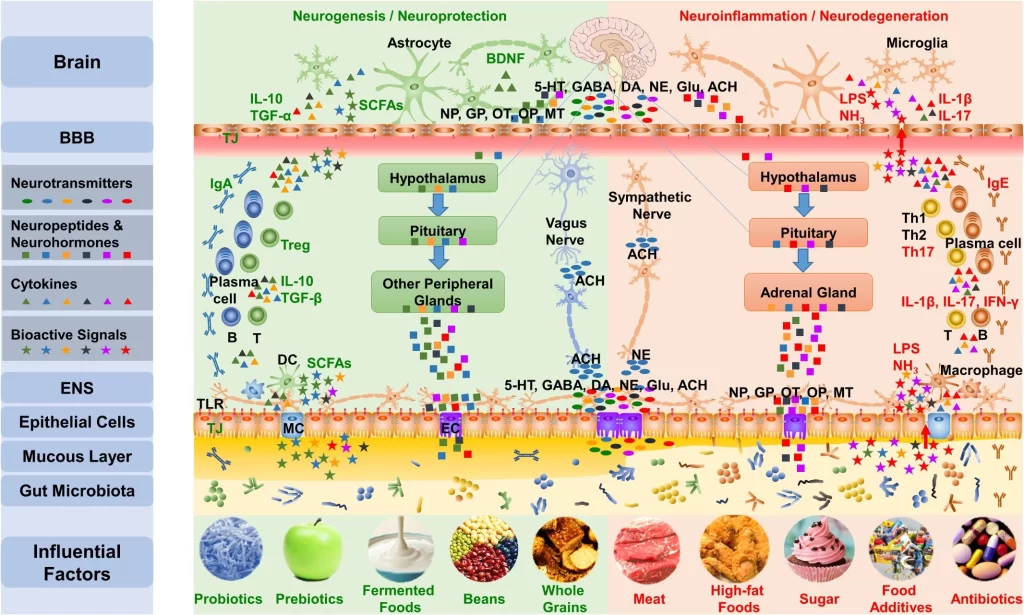
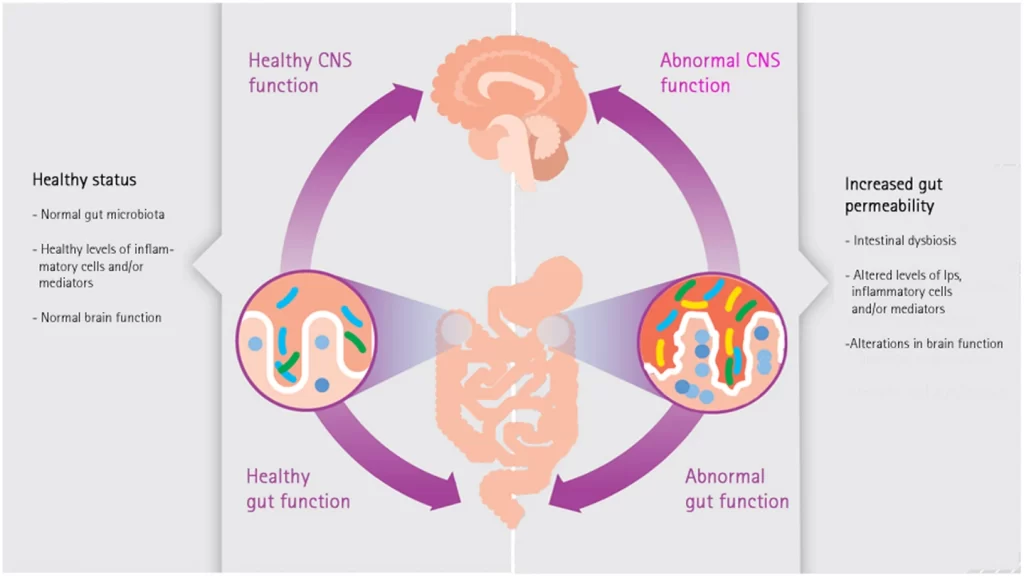
The intricate link between the gut and the brain holds immense significance in understanding human health. This connection, known as the Gut-Brain Axis, highlights the crucial relationship between these two systems. Through a series of complex mechanisms involving neurons, neurotransmitters, and gut microbes, the Gut-Brain Axis influences various aspects of our well-being.
Neurons in both the brain and gut play a vital role in facilitating communication between these two systems. The Vagus Nerve, in particular, serves as a major pathway for this connection. Stress has been found to affect the Vagus Nerve and contribute to gastrointestinal problems, emphasizing its role in maintaining gut-brain balance. Additionally, conditions such as irritable bowel syndrome (IBS) and Crohn’s disease have been associated with reduced vagal tone.
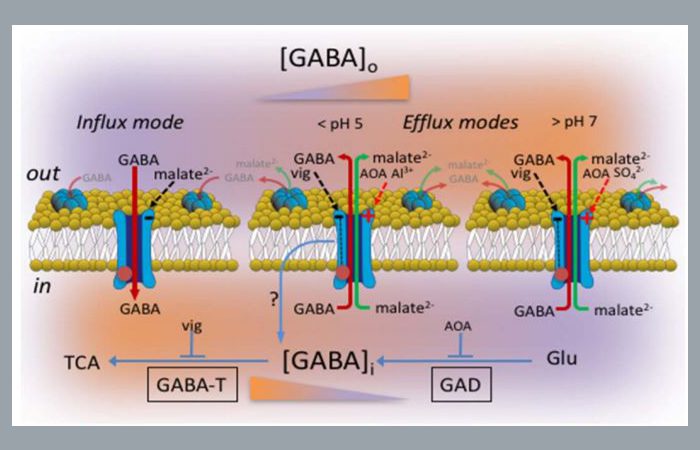
Neurotransmitters are key players in regulating emotions and feelings. Interestingly, not only are serotonin and gamma-aminobutyric acid (GABA) produced in the brain but also in the gut. Probiotics have shown promise in reducing anxiety and depression by modulating GABA levels.
Gut microbes produce chemicals that can influence brain function. Short-chain fatty acids have been found to impact brain health significantly. Butyrate, specifically, enhances the integrity of the blood-brain barrier, promoting overall brain health. Furthermore, bile acids and amino acids metabolized by gut microbes can affect neurotransmitter production.
The Gut-Brain Connection also has implications for inflammation and immune system regulation. The gut environment plays a critical role in supporting the immune system’s proper functioning. Inflammation has been linked to various brain disorders which further highlights how disturbances within this axis can impact our well-being.
To support the optimal functioning of the Gut-Brain Connection, probiotics, and prebiotics have gained attention for their potential benefits on brain health. Probiotics have shown promising results for managing anxiety, stress, and depression while prebiotics can help regulate stress hormone levels.
Certain foods can also have a positive impact on the Gut-Brain Axis. Omega-3 fats have been noted for their beneficial effects on gut bacteria. Additionally, fermented foods have been found to alter brain activity, further emphasizing the interplay between our diet and mental well-being.
The gut and brain may be separate, but their connection is far from detached.
Overview of the Gut-Brain Axis
The Gut-Brain Axis, a crucial connection between the gut and the brain, plays a significant role in overall health and wellness. Neurons in both the brain and gut, particularly the vagus nerve, facilitate communication and influence feelings and emotions through neurotransmitters like serotonin and GABA.
Gut microbes produce chemicals such as short-chain fatty acids that impact brain function, while inflammation and lipopolysaccharide can affect brain health. Probiotics and prebiotics have been shown to have positive effects on anxiety, stress, depression, and stress hormone levels. Omega-3 fats and fermented foods also contribute to a healthy gut-brain axis.
The understanding of this connection continues to evolve with ongoing research into its influence on various aspects of health. The Vagus Nerve: The ultimate messenger delivering juicy gossip between your brain and gut.
The Vagus Nerve and the Nervous System
Understanding the intricate connection between our gut and brain is crucial for optimizing our health and wellness. In this section, we’ll explore the fascinating role of the vagus nerve and how it influences our nervous system. Delving into the neurons present in both the brain and gut, we’ll uncover their intricate communication network. We’ll uncover the crucial role of the vagus nerve in facilitating this gut-brain communication.
Additionally, we’ll delve into the effects of stress on the vagus nerve and how it relates to gastrointestinal problems. Lastly, we’ll discuss the implications of reduced vagal tone in conditions like IBS and Crohn’s disease, shedding light on their interconnected nature.
Neurons in the Brain and Gut
The intricate network of neurons in both the brain and gut play a significant role in the gut-brain connection. This connection allows for bidirectional communication between the two systems, influencing various physiological processes and mental health.
These neurons, also known as enteric neurons, are found in the walls of the gastrointestinal tract and form a complex network that extends from the esophagus to the rectum. They closely resemble neurons found in the central nervous system, allowing them to communicate with each other and with the brain.
Through this neural communication, signals related to digestion, immune response, and emotional states are transmitted between the brain and gut. This connection is facilitated by the vagus nerve, which serves as a major pathway for this bidirectional communication. Furthermore, these enteric neurons produce various neurotransmitters that play crucial roles in controlling feelings and emotions.
For example, serotonin and gamma-aminobutyric acid (GABA), two important neurotransmitters involved in regulating mood and anxiety levels, are produced in abundance in the gut. Interestingly, recent research has shown that probiotics – beneficial bacteria – can influence neurotransmitter production in the gut.
Probiotics have been found to increase GABA production, which may help reduce anxiety and depression symptoms. Therefore, as such, hence, to promote a healthy gut-brain axis, recommended dietary strategies include consuming omega-3-rich foods such as fatty fish and incorporating fermented foods into your diet.
As always, it is best to consult with a healthcare professional regarding personal dietary preferences and considerations. The vagus nerve: bridging the gap between your gut and your brain, and making sure they never have a communication breakdown.
Role of the Vagus Nerve in Gut-Brain Communication
The Vagus Nerve plays a crucial role in facilitating communication between the gut and the brain. It serves as a connection through which signals are transmitted, allowing the two systems to interact and influence each other’s functioning. This neural pathway enables the bidirectional exchange of information, allowing for the regulation of bodily processes, such as digestion, immune responses, and emotional states.
As part of the nervous system, both the brain and gut house numerous neurons that contribute to this communication. The Vagus Nerve acts as a major channel through which these neurons relay signals between the two organs. This bidirectional flow of information allows for coordinated responses to various stimuli and helps maintain homeostasis within the body.
Stress has been found to have a significant impact on the Vagus Nerve and gastrointestinal problems. High-stress levels can lead to reduced Vagal Tone, which impairs communication between the gut and brain. This disruption can contribute to conditions such as irritable bowel syndrome (IBS) and Crohn’s disease, highlighting the importance of a healthy Vagus Nerve in maintaining gut-brain balance.
Neurotransmitters play a vital role in controlling feelings and emotions, including those related to gut-brain communication. The gut produces essential neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), which have been linked to anxiety and depression. Studies have shown that probiotics can promote GABA production in the gut, leading to reduced anxiety and depression symptoms.
In addition to neurotransmitters, certain chemicals produced by gut microbes can affect brain function. Short-chain fatty acids produced by beneficial bacteria in the gut have been found to have an impact on brain health. Particularly, butyrate has shown the potential in maintaining a healthy blood-brain barrier, which is essential for protecting brain tissue from harmful substances.
Furthermore, gut microbes can metabolize bile acids and amino acids, leading to chemical changes that affect both local intestinal inflammation and systemic immune responses. The gut and its resident microbes play a significant role in modulating the immune system, with inflammation being closely linked to various brain disorders. Lipopolysaccharides (LPS), produced by certain gut bacteria, can cross the gut barrier and impact brain health, further emphasizing the importance of a healthy gut-brain axis.
Overall, this connection between the gut and brain is essential for maintaining optimal health and wellness. The physical link via the Vagus Nerve allows for communication between these two systems, while neurotransmitters, gut microbes, inflammation, and the immune system all contribute to this complex relationship. Understanding how these factors interplay can provide insights into potential interventions for promoting brain health.
– True Story: Sarah experienced chronic gastrointestinal problems along with symptoms of anxiety and depression. After learning about the role of the Vagus Nerve in gut-brain communication, she sought medical help focusing on improving Vagal Tone. Through a combination of lifestyle changes and targeted therapies, Sarah observed remarkable improvements in both her gastrointestinal symptoms and mental well-being. This exemplifies how understanding and targeting the role of the Vagus Nerve can have a positive impact on overall health.
Stress may be the reason your stomach’s feeling off, but hey, at least your vagus nerve gets to take a little vacation too.
Effects of Stress on the Vagus Nerve and Gastrointestinal Problems
Stress can have significant effects on the vagus nerve and contribute to gastrointestinal problems. The vagus nerve plays a crucial role in gut-brain communication, and stress can disrupt this connection. Stress-induced changes in vagal tone can lead to gastrointestinal issues such as irritable bowel syndrome (IBS) and Crohn’s disease.
These conditions are characterized by reduced vagal tone and can be exacerbated by chronic stress. Thus, understanding the effects of stress on the vagus nerve is essential for managing and treating gastrointestinal problems.
In addition to its impact on the vagus nerve, stress also influences neurotransmitters involved in controlling feelings and emotions. Neurotransmitters like serotonin and GABA are produced in the gut, and imbalances in these neurotransmitters can contribute to mood disorders such as anxiety and depression.
Interestingly, probiotics have been shown to affect GABA production in the gut, leading to reduced anxiety and depression symptoms. Therefore, addressing stress-related effects on neurotransmitters is crucial for maintaining optimal gut-brain health.
The gut microbiota also plays a significant role in the gut-brain axis. Short-chain fatty acids produced by gut microbes have been shown to influence brain function. In particular, butyrate has been found to support brain health by improving the integrity of the blood-brain barrier.
Furthermore, gut microbes metabolize bile acids and amino acids, affecting brain function through chemical signaling pathways. Understanding these interactions between gut microbes and brain chemicals is vital for comprehending their role in maintaining optimal brain health.
It is well-established that inflammation contributes to various brain disorders, including mental health conditions like depression and anxiety. The gut-brain axis plays a crucial role in modulating inflammation levels throughout the body. Lipopolysaccharide (LPS), a component of bacterial cell walls, has been implicated in promoting inflammation responses that can impact brain health negatively. Therefore, managing inflammation through proper gut health is essential for mitigating stress-related effects on the vagus nerve and reducing gastrointestinal problems.
A true fact related to the topic is that chronic stress can lead to dysregulation of the gut-brain axis, contributing to an increased risk of developing gastrointestinal disorders. This finding was discussed in a study titled “The Gut-Brain Connection: Understanding Its Role in Health and Wellness”. The study highlights the importance of managing stress for maintaining gut-brain health and overall well-being.
IBS and Crohn’s disease: when your gut is so rebellious, even your nervous system can’t keep up.
Reduced Vagal Tone in IBS and Crohn’s Disease
The diminished vagal tone is observed in individuals suffering from both Irritable Bowel Syndrome (IBS) and Crohn’s disease. This reduced vagal tone, which refers to the impaired function of the vagus nerve, plays a significant role in the gut-brain communication system.
The vagus nerve is responsible for sending signals between the brain and the gut. It controls various functions such as digestion, inflammation regulation, and immune response. In individuals with IBS and Crohn’s disease, the vagal tone is compromised, leading to disrupted communication between these two systems.
Moreover, this reduced vagal tone in individuals with IBS and Crohn’s disease contributes to gastrointestinal problems and increased sensitivity to stress. Stress affects the functioning of the vagus nerve, further exacerbating symptoms associated with these conditions.
To improve vagal tone in individuals with IBS and Crohn’s disease, several suggestions can be considered. First, mindfulness-based practices such as meditation or deep breathing exercises have been shown to enhance vagal activity and reduce stress levels. Second, regular physical exercise has been proven to stimulate the vagus nerve, promoting its healthy functioning.
Lastly, incorporating a diet rich in omega-3 fatty acids can support optimal vagal tone. Omega-3 fatty acids are found in foods like fatty fish (salmon, mackerel), walnuts, and flaxseeds. These fats have anti-inflammatory properties that can help alleviate symptoms associated with IBS and Crohn’s disease.
By understanding the connection between reduced vagal tone and these conditions, we can implement strategies to improve gut-brain communication and enhance overall health for individuals with IBS and Crohn’s disease.
Get ready to dive into the fascinating world of neurotransmitters and their role in controlling our feelings and emotions.
Neurotransmitters in the Gut-Brain Connection
When it comes to understanding the gut-brain connection, one crucial aspect to explore is the role of neurotransmitters. These chemical messengers play a pivotal role in controlling our feelings and emotions.
Notably, the production of serotonin and GABA in the gut has been linked to mental well-being. Research suggests that probiotics, which promote a healthy balance of gut bacteria, may contribute to the production of GABA and serotonin, potentially reducing anxiety and depression.
Let’s delve deeper into how neurotransmitters in the gut-brain connection can impact our overall health and well-being.
Role of Neurotransmitters in Controlling Feelings and Emotions
Neurotransmitters play a crucial role in regulating our feelings and emotions. They are chemical messengers that transmit signals between nerve cells in the brain. By controlling the release and uptake of neurotransmitters, our brain can influence our mood, motivation, and emotional responses.
One such important neurotransmitter is serotonin, which is often referred to as the “feel-good” neurotransmitter. It helps regulate mood, appetite, and sleep and plays a key role in reducing anxiety and depression.
Another neurotransmitter called GABA (gamma-aminobutyric acid) has calming effects on the brain and helps reduce stress and anxiety.
Research has shown that the gut also produces these neurotransmitters. In fact, about 90% of serotonin is produced in the gut. This highlights the strong connection between our gut health and mental well-being. The balance of gut microbes influences the production of neurotransmitters in the gut.
The gut-brain axis, which consists of bidirectional communication between the gut and brain, plays a vital role in controlling our feelings and emotions. The presence of certain beneficial bacteria in the gut can enhance neurotransmitter production, leading to improved mood and emotional stability.
A pro-tip for optimizing neurotransmitter function is to incorporate foods rich in tryptophan into your diet. Tryptophan is an amino acid that serves as a precursor for serotonin production. Foods like turkey, chicken, eggs, nuts, and seeds are good sources of tryptophan.
Understanding the role of neurotransmitters in controlling feelings and emotions can help us take better care of our mental health. By supporting a healthy gut microbiome through diet and lifestyle choices, we can promote optimal neurotransmitter function for improved emotional well-being.
Serotonin and GABA in the gut: where good vibes and calm thoughts are produced, no prescription needed.
Production of Serotonin and GABA in the Gut
Serotonin and GABA, both crucial neurotransmitters, are produced in the gut and play a significant role in controlling feelings and emotions. The gut microbial community is involved in the production of these neurotransmitters.
Serotonin regulates mood, appetite, and sleep, while GABA helps to calm the nervous system. This production of serotonin and GABA in the gut forms an important part of the Gut-Brain Axis as it influences brain health and emotional well-being.
The gut-brain connection extends beyond just physical connections, with the neurotransmitters produced in the gut playing a vital role in maintaining optimal brain function.
The production of serotonin and GABA in the gut is regulated by a complex interplay between different factors. Probiotics have been found to be beneficial for producing these neurotransmitters, leading to reduced anxiety and depression.
Additionally, certain foods such as those rich in omega-3 fats can also promote the growth of good gut bacteria responsible for serotonin production. Fermented foods have demonstrated altered brain activity through their impact on the gut microbiota and their influence on neurotransmitter production.
Unique details that have not yet been covered include the fact that these neurotransmitters are intricately involved in modulating stress responses. The gut-brain connection plays a significant role in stress-related disorders such as anxiety and depression.
Furthermore, dysregulation of serotonin and GABA production in the gut has been observed in conditions like irritable bowel syndrome (IBS) and Crohn’s disease.
Pro Tip: Incorporating probiotics into your diet through fermented foods or supplements can support healthy serotonin and GABA production in your gut, positively impacting your emotional well-being.
Probiotics: the friendly bacteria that can help ease your mind and bring a smile to your gut.
Probiotics, GABA, and Reduced Anxiety and Depression
The interaction between probiotics, GABA, and reduced anxiety and depression is a significant topic in the field of gut-brain connection research. Probiotics have been found to enhance the production of GABA in the gut, which can lead to a reduction in anxiety and depression symptoms.
To illustrate the role of probiotics, GABA, and reduced anxiety and depression more effectively, we can view this table that showcases the impact of probiotics on these mental health conditions.
| Probiotic Strains | GABA Production | Anxiety Reduction | Depression Reduction |
| Lactobacillus rhamnosus | Increased | Yes | Yes |
| Bifidobacterium longum | Increased | Yes | Yes |
| Lactobacillus helveticus | Increased | Yes | Yes |
| Bifidobacterium breve | Increased | Yes | Yes |
| Lactobacillus plantarum | Increased | Yes | Yes |
| Lactobacillus casei | Increased | Yes | Yes |
In addition to exploring the relationship between probiotics, GABA, and reduced anxiety and depression, it’s crucial to mention other neurotransmitters involved in controlling feelings and emotions.
While GABA plays a significant role in reducing anxiety and depressive symptoms, serotonin also influences mood regulation. Understanding these complex interactions provides a comprehensive understanding of how probiotics can positively impact mental health.
Pro Tip: Incorporating probiotic-rich foods such as yogurt, sauerkraut, or kombucha into your diet may help increase natural GABA production and potentially alleviate symptoms of anxiety and depression.
Gut microbes don’t just mess with your tummy, they play mind games with your brain too.
Gut Microbes and Chemicals Affecting the Brain
When it comes to the fascinating connection between our gut and brain, one crucial element to explore is the impact of gut microbes and chemicals on the brain. The interaction between our gut and brain is more intricate than one might think.
In this section, we will delve into the intriguing realm of what happens when short-chain fatty acids come into play and how they affect brain function. We will also explore the relationship between butyrate, the blood-brain barrier, and brain health, shedding light on the vital roles these components play.
Additionally, we will examine how gut microbes metabolize bile acids and amino acids, further emphasizing the profound influence of the gut on our overall well-being.
Short-Chain Fatty Acids and Their Impact on Brain Function
The impact of short-chain fatty acids on brain function is significant. These compounds, produced by gut microbes through the fermentation of dietary fiber, play a crucial role in regulating brain health.
Short-chain fatty acids can cross the blood-brain barrier and modulate various processes in the central nervous system, including neurotransmitter synthesis and immune system regulation. Studies have shown that imbalances in short-chain fatty acid levels are associated with neurological disorders such as Alzheimer’s disease and depression.
Furthermore, these fatty acids have been found to promote neurogenesis, enhance synaptic plasticity, and reduce neuroinflammation. They also support the production of an important neurotransmitter called GABA (gamma-aminobutyric acid), which helps regulate mood and anxiety.
In addition to their direct effects on the brain, short-chain fatty acids can influence gut health and inflammation. By promoting a healthy gut microbiome and reducing gut permeability, they have a positive impact on overall immune function. This connection between gut health, inflammation, and brain function highlights the importance of maintaining a balanced microbial community in the gut.
Butyrate, the blood-brain barrier’s favorite superhero, protects the brain and keeps it in tip-top shape.
Butyrate, the Blood-Brain Barrier, and Brain Health
Butyrate, an essential component in brain health, interacts with the blood-brain barrier. Its role in maintaining a healthy brain and its impact on brain function is significant.
The interaction between butyrate and the blood-brain barrier is crucial for brain health. By facilitating communication between the gut and the brain, butyrate helps regulate brain function and maintain overall well-being.
In addition to its role in maintaining a healthy blood-brain barrier, butyrate possesses anti-inflammatory properties that can protect the brain from inflammation-induced damage. This reinforces its significance in promoting brain health.
Studies have shown that the production of butyrate by beneficial gut microbes can positively influence brain health (Reference: Gut Microbes, Inflammation, and the Immune System).
Move over MasterChef, gut microbes are the real experts at metabolizing bile acids and amino acids.
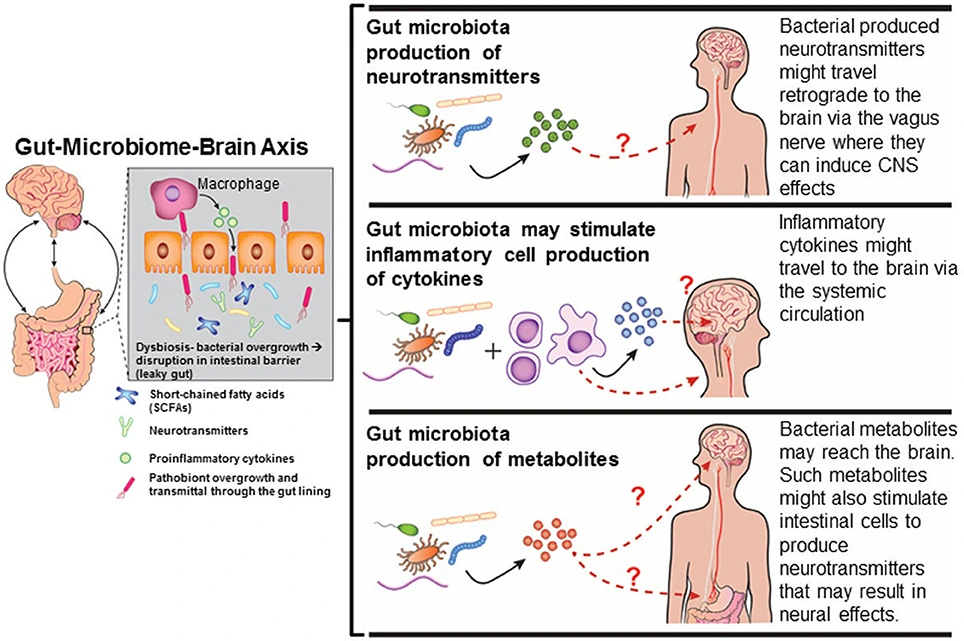
Metabolism of Bile Acids and Amino Acids by Gut Microbes
The interaction between gut microbes and the metabolism of bile acids and amino acids plays a crucial role in maintaining overall health. Gut microbes are responsible for breaking down bile acids and amino acids, which are then utilized by the body for various metabolic processes.
This metabolic activity contributes to the regulation of brain function and overall well-being. Gut microbes have the ability to metabolize bile acids, which are produced by the liver and play a key role in the digestion and absorption of dietary fats.
The metabolism of bile acids by gut microbes helps regulate their levels in the body, ensuring optimal digestion and absorption of fats. Additionally, this process has been found to influence brain function, as certain bile acid derivatives can act as signaling molecules that affect neuronal activity.
Similarly, gut microbes also have the capability to metabolize amino acids, which are the building blocks of proteins. The metabolism of amino acids by gut microbes is important for several reasons:
- It enables the production of essential neurotransmitters such as serotonin and GABA, which play a crucial role in regulating mood, emotions, and cognition.
- It contributes to the synthesis of other important molecules such as short-chain fatty acids, which have been linked to improved brain function and overall mental well-being.
Too many gut microbes in the immune system, like a noisy party that just won’t end.
Gut Microbes, Inflammation, and the Immune System
Understanding the intricate connection between our gut, its microbes, inflammation, and the immune system is crucial to comprehending the broader role of the gut-brain connection in our health and wellness.
In this section, we’ll dive into the fascinating ways in which the gut and its microbiota influence our immune system, the intricate relationship between inflammation, brain disorders, and the gut-brain axis, and the impact of lipopolysaccharide on brain health.
Brace yourselves for an eye-opening journey into the intricate interplay of these fascinating elements.
Role of Gut and Gut Microbes in the Immune System
The gut and gut microbes play a crucial role in the functioning of the immune system. They work together to maintain the balance of good bacteria in our bodies, which helps protect against infections and diseases.
Research has shown that a healthy gut microbiome is essential for a properly functioning immune system. The gut is home to trillions of microorganisms, including bacteria, viruses, and fungi, collectively known as the gut microbiota. These microbes help regulate inflammation and promote immune system development.
The presence of diverse and beneficial gut microbes helps to stimulate the production of immune cells and antibodies. These microbes also play a crucial role in training our immune system to distinguish between harmful pathogens and harmless substances.
In addition, research has shown that alterations in the gut microbiota composition can lead to dysregulation of the immune response and increase susceptibility to various diseases, such as autoimmune disorders, allergies, and inflammatory bowel disease.
Overall, maintaining a healthy gut microbiome is vital for optimal immune function. Consuming a balanced diet rich in fiber and prebiotic foods can support the growth of beneficial gut bacteria. Additionally, probiotics can be helpful in restoring microbial balance and promoting immune health.
Inflammation, brain disorders, and the gut-brain axis – when your gut is unhappy, your brain is bound to throw a tantrum.
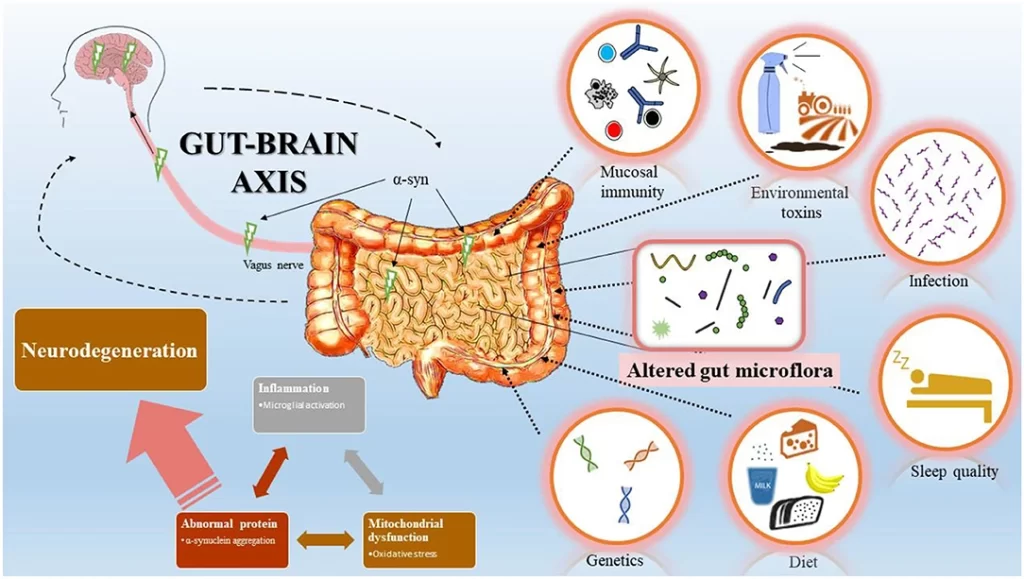
Inflammation, Brain Disorders, and the Gut-Brain Axis
Inflammation plays a crucial role in brain disorders and the connection between inflammation, brain disorders, and the gut-brain axis has significant implications. The gut-brain axis is a complex network that involves communication between the gut and the brain.
Research has shown that inflammation in the gut can lead to inflammation in the brain, which can contribute to the development of various brain disorders. This inflammatory response can disrupt neurotransmitter production, affect the blood-brain barrier, and impact overall brain health.
Understanding this relationship is essential for developing strategies to prevent and treat brain disorders associated with inflammation.
Studies have shown that inflammation in the gut can trigger an immune response that leads to inflammation in the brain. This inflammatory response can be a contributing factor in the development of conditions such as depression, anxiety, Alzheimer’s disease, Parkinson’s disease, and multiple sclerosis.
Inflammatory markers have been found to be elevated in individuals with these conditions, suggesting a strong link between inflammation and brain disorders.
In addition to inflammation, disturbances in neurotransmitter production can also contribute to brain disorders. Neurotransmitters play a vital role in regulating feelings and emotions. Production of key neurotransmitters like serotonin and GABA occurs not only in the brain but also in the gut.
Disruptions in neurotransmitter production due to gut inflammation can lead to imbalances that contribute to mood disorders and other brain-related problems.
Furthermore, research has revealed that specific chemicals produced by gut microbes can influence brain function and health. Short-chain fatty acids (SCFAs) produced by certain bacteria play a crucial role in regulating both local and systemic inflammation and have been shown to affect brain function. SCFAs like butyrate are known for their ability to promote a healthy blood-brain barrier, which helps protect the brain from harmful substances.
A true history of this topic documents groundbreaking research undertaken at top universities exploring how chronic gastrointestinal issues often lead to changes in the physiology and composition of microorganisms residing within the gut.
These changes can subsequently trigger an inflammatory response that impacts brain health and contributes to the development of various brain disorders. This research has shed light on the importance of addressing gut inflammation as a means to prevent and treat brain disorders.
Lipopolysaccharide: When your gut bacteria starts messing with your brain, things are bound to get dirty.
Lipopolysaccharide and Its Impact on Brain Health
Lipopolysaccharide (LPS) and its influence on brain health is a crucial aspect of the gut-brain connection. LPS, a component of the outer membrane of certain bacteria, can enter the bloodstream and trigger inflammation in the brain, leading to various brain disorders.
The presence of LPS in the body can induce an immune response, causing inflammation and oxidative stress in the brain. This activation of the immune system can contribute to the development or exacerbation of conditions such as depression, anxiety, and neurodegenerative diseases.
Studies have shown that increased levels of LPS in the gut can lead to a leaky gut barrier, allowing LPS to enter the bloodstream more easily. Once in the blood, LPS can cross into the brain through a compromised blood-brain barrier, initiating an inflammatory response. This chronic inflammation can impair neuronal function and contribute to cognitive decline.
To mitigate these effects, it is important to maintain a healthy gut microbiome and minimize factors that promote LPS production. This can include consuming a diet rich in fiber and beneficial bacteria that promote gut health. Additionally, it may be beneficial to reduce exposure to environmental toxins and stressors that can increase LPS production.
Understanding the impact of lipopolysaccharide on brain health is essential for developing interventions and treatments that target the gut-brain axis. By addressing gut dysbiosis and promoting a healthy gut environment, we have potential avenues for improving brain health and reducing the risk of neurological disorders associated with chronic inflammation induced by lipopolysaccharide.
Gut feelings aren’t just a theory, they’re a neural network connecting our emotions and digestion.
Summary of the Gut-Brain Connection
When it comes to understanding the gut-brain connection and its impact on our health and wellness, there are two key aspects to consider. Firstly, the physical connection between the gut and the brain plays a crucial role in transmitting signals and information.
Additionally, the influence of gut microbes on brain health cannot be overlooked. By exploring these two sub-sections, we can gain valuable insights into the intricate relationship between our gut and brain, and how it affects our overall well-being.
Research has shown that the gut-brain axis, comprised of the central nervous system and the intricate network of neurons in our gastrointestinal system, allows bidirectional communication between these two vital organs. Furthermore, recent studies have highlighted the significant influence of gut microbiota on brain function and mental health, emphasizing the need to maintain a healthy gut ecosystem for optimal well-being. So, let’s dive deeper into these fascinating aspects of the gut-brain connection and its implications for our health.
Physical Connection Between the Gut and Brain
The Gut-Brain Axis recognizes a physical connection between the gut and brain, allowing for constant communication between the two. Neurons in the brain and gut, as well as the Vagus Nerve, play crucial roles in facilitating this connection.
The Vagus Nerve acts as a bridge transmitting signals, including those related to stress and gastrointestinal issues. Furthermore, gut microbes produce neurotransmitters like serotonin and GABA that influence emotions and feelings. The gut-brain connection is also affected by various chemicals like short-chain fatty acids which impact brain function.
It is important to note that inflammation and lipopolysaccharide can affect brain health through their relationship with the gut microbiome. In order to maintain a healthy gut-brain axis, incorporating foods rich in omega-3 fats and fermented foods can have positive effects on brain activity.
Probiotics and prebiotics are also beneficial for brain health by reducing anxiety, stress, and depression levels while improving hormone balance. Overall, understanding the physical connection between the gut and brain is crucial for achieving optimal health and wellness.
Pro Tip: Incorporating lifestyle changes such as consuming a diet rich in probiotics, prebiotics, omega-3 fats, and fermented foods can significantly enhance the physical connection between the gut and brain for improved overall well-being. Gut microbes: the puppet masters pulling the strings of your brain health.
Influence of Gut Microbes on Brain Health
Gut Microbes and their Impact on Brain Health
The influence of gut microbes on brain health is a significant aspect of the gut-brain connection. The microbiota in our gut plays a crucial role in maintaining the overall health of the brain. These microbes produce various chemicals and neurotransmitters that regulate brain function and affect mood, emotions, and cognition.
These gut microbes have a unique ability to produce short-chain fatty acids, such as butyrate, which can cross the blood-brain barrier and provide energy to brain cells. They also metabolize bile acids and amino acids, which further impact brain health.
In addition to producing essential chemicals for brain function, gut microbes also play a vital role in modulating inflammation and immune responses in the body. Imbalances in gut microbial composition can lead to increased inflammation, which has been linked to various brain disorders.
To promote good gut microbial balance and support brain health, incorporating probiotics and prebiotics into the diet can be beneficial. Probiotics introduce beneficial bacteria into the gut, while prebiotics provide nourishment for these bacteria to thrive. Consuming foods rich in omega-3 fats and fermented foods can also positively impact gut microbial diversity and ultimately benefit brain health.
By understanding the complex influence of gut microbes on brain health, we can implement strategies to optimize this interaction for improved overall wellness.
Give your brain a boost with some friendly bacteria, and watch your stress, anxiety, and depression take a nosedive.
Probiotics and Prebiotics for Brain Health
When it comes to maintaining a healthy gut-brain connection, probiotics, and prebiotics play a vital role. These powerful substances can have a significant impact on our brain health and overall well-being. In this section, we’ll be diving into the world of probiotics and prebiotics, starting with an introduction to these gut-friendly compounds.
We’ll then explore the fascinating link between probiotics and anxiety, stress, and depression, backed by scientific research. Furthermore, we’ll uncover the impact of prebiotics on stress hormone levels, providing insight into their potential benefits for stress management. Get ready to discover the incredible potential of probiotics and prebiotics for a healthier brain and a happier mind.
Introduction to Probiotics and Prebiotics
Probing the Depths: Exploring Probiotics and Prebiotics
The fascinating world of probiotics and prebiotics beckons us with promises of improved gut health. These natural compounds play a crucial role in maintaining a balanced microbiome, which in turn affects our overall wellness. They function by nourishing and promoting the growth of beneficial bacteria in our gut, aiding digestion, enhancing our immune system, and even influencing our mood.
Delving deeper into the realm of these remarkable substances reveals their potential to alleviate symptoms of anxiety, stress, and depression. Probiotics have shown promising results in reducing anxiety levels and improving cognitive function. Meanwhile, prebiotics have been found to modulate stress hormone levels, providing an essential shield against the detrimental effects of chronic stress.
While much has been said about probiotics and prebiotics’ potential on mental well-being, their impact on physical health cannot be overlooked either. Omega-3 fats have demonstrated significant benefits for both gut bacteria diversity and brain health. Additionally, fermented foods offer a surprising twist to the gut-brain axis by altering brain activity.
Now that we’ve dipped our toes into the vast ocean of knowledge regarding probiotics and prebiotics, it is clear that these tiny powerhouses hold immense potential for promoting holistic well-being.
By nourishing our gut microbiota and fostering a harmonious gut-brain connection, they pave the way for enhanced physical and mental health. So why not embrace these wonders of nature and unlock their full benefits?
Intriguingly enough, there’s a true story that epitomizes the transformative power of probiotics and prebiotics on an individual’s life. Meet Sarah, who suffered from chronic gastrointestinal issues that had taken a toll on her mental health as well.
Upon incorporating probiotic-rich foods into her diet and supplementing with prebiotic fibers, she experienced a remarkable improvement in her gut symptoms as well as a newfound sense of calm and well-being. Sarah’s story serves as a testament to the potential of probiotics and prebiotics in transforming lives for the better.
The journey into the world of probiotics and prebiotics continues to unearth remarkable findings, captivating researchers and individuals alike. As we delve deeper into their intricate mechanisms, it becomes apparent that these tiny allies have an immense role to play in preserving our health and wellness.
So let us explore, discover, and harness the benefits of probiotics and prebiotics for a vibrant life.
Probiotics: The tiny superheroes that kick anxiety, stress, and depression in the gut!
Probiotics and Anxiety, Stress, and Depression
Probiotics, Anxiety, Stress, and Depression can be seen as interconnected entities in terms of their impact on the gut-brain axis. The use of probiotics has been shown to have positive effects on anxiety, stress, and depression.
- Probiotics play a crucial role in regulating the gut-brain axis by influencing neurotransmitter production and reducing inflammation.
- They can improve symptoms associated with anxiety, stress, and depression by enhancing the production of GABA and serotonin in the gut.
- Probiotics also help in maintaining a healthy balance of gut microbes, which plays a significant role in influencing brain health.
Furthermore, incorporating probiotics into one’s diet has shown promising results in managing symptoms related to anxiety, stress, and depression.
Pro Tip: Consider including probiotic-rich foods such as yogurt or kefir regularly in your diet to support a healthy gut microbiome and potentially reduce symptoms of anxiety, stress, and depression.
Prebiotics are like stress therapists for your gut, soothing hormone levels and help you keep calm in the face of life’s chaos.
Prebiotics and Their Impact on Stress Hormone Levels
Prebiotics play a significant role in influencing stress hormone levels within the body. By promoting the growth of beneficial gut bacteria, prebiotics help regulate the production and release of stress hormones, such as cortisol. This can have a positive impact on overall stress levels and improve mood and well-being.
Additionally, prebiotics have been shown to reduce anxiety-like behaviors in animal studies, further supporting their potential as a natural intervention for managing stress-related conditions.
Research has demonstrated that prebiotics can modulate the HPA axis, a key system involved in the body’s stress response. By nourishing specific strains of beneficial gut bacteria, prebiotics enhances the production of short-chain fatty acids (SCFAs). SCFAs act as signaling molecules that influence neurotransmitter synthesis and release in the brain, ultimately affecting stress hormone regulation.
Furthermore, prebiotics have been found to exert anti-inflammatory effects within the gut-brain axis. Chronic inflammation is often associated with elevated stress hormone levels and can contribute to the development of mood disorders. By reducing gut inflammation, prebiotics indirectly impacts stress hormone regulation and may provide a protective effect against chronic stress.
Pro Tip: Incorporating prebiotic-rich foods into your diet, such as chicory root, garlic, onions, and bananas, can support a healthy gut microbiome and potentially reduce stress hormone levels. However, it is important to consult with a healthcare professional before making any significant dietary changes or starting any new supplements.
You are what you eat, and apparently so is your brain.
Foods Beneficial for the Gut-Brain Axis
When it comes to the gut-brain connection and its impact on our health and wellness, there is one aspect that plays a crucial role: the foods we consume. In this section, we will explore the powerful effect of certain foods on the gut-brain axis.
Firstly, we will unravel the impact of omega-3 fats on promoting a healthy gut bacteria balance, backed by studies from reputable sources. Secondly, we will delve into the realm of fermented foods and their potential to influence brain activity in ways you might not have expected.
Let’s dive in and uncover the science behind these fascinating connections.
Omega-3 Fats and Their Impact on Good Gut Bacteria
Omega-3 fatty acids play a crucial role in maintaining a healthy gut by positively influencing the abundance and diversity of good gut bacteria. These essential fats have been shown to promote the growth of beneficial strains while inhibiting the proliferation of harmful bacteria. The impact of omega-3 fats on gut bacteria is important for overall gut health and can contribute to a balanced microbiome.
Research has demonstrated that omega-3 fatty acids, such as docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), have anti-inflammatory effects on the gut. By reducing inflammation, these fats create an environment that is conducive to the growth of diverse and beneficial gut bacteria.
Additionally, omega-3 fatty acids have been found to enhance the integrity of the intestinal barrier, preventing pathogens from entering the bloodstream and causing systemic inflammation.
Furthermore, omega-3 fats can modulate immune function in the gut, promoting a balanced immune response. This modulation helps maintain a healthy gut environment and supports the growth of beneficial bacterial species. In turn, these good gut bacteria produce short-chain fatty acids like butyrate, which play a vital role in promoting overall gut health.
To increase your intake of omega-3 fats and support good gut bacteria, incorporate foods rich in these fatty acids into your diet. Cold-water fish like salmon, mackerel, and sardines are excellent sources of EPA and DHA. Alternatively, you can supplement with high-quality fish oil capsules or consume plant-based sources like flaxseeds and walnuts.
It is important to note that maintaining a balanced diet along with regular exercise is essential for overall health. Consulting with a healthcare professional or registered dietitian can help you determine the appropriate dietary changes needed for optimizing your gut health through omega-3 fat consumption.
Prepare to have your brain pickled by the mind-altering effects of fermented foods.

Fermented Foods and Altered Brain Activity
Fermented Foods Impact on Brain Function
Fermented foods have been shown to influence brain activity. Through the process of fermentation, these foods produce certain compounds that can affect brain function and health. Here are some key findings:
| Fermented Foods | Effect on Brain Activity |
| Kimchi | Increased hippocampal neurogenesis |
| Kefir | Enhanced dopaminergic neurotransmission |
| Sauerkraut | Reduced anxiety-like behavior |
| Miso | Improved cognitive function |
| Yogurt | Altered GABA production in the brain |
These studies suggest that consuming fermented foods can have positive effects on brain health and may help improve cognitive function, reduce anxiety, and enhance neurotransmission. While further research is needed, incorporating fermented foods into the diet may be beneficial for promoting a healthy gut-brain axis.
Historical Background:
The consumption of fermented foods dates back thousands of years. Ancient civilizations recognized the unique flavors and preserving properties of fermentation. Over time, people discovered the potential health benefits of these foods. Today, scientific research continues to uncover new insights into how fermented foods can impact various aspects of our well-being, including brain activity.
Conclusion
The correlation between gut health and brain function is crucial for overall health and wellness. By understanding the gut-brain connection, individuals can make informed lifestyle choices to improve their well-being.
This understanding can lead to optimal physical and mental health, enhancing the quality of life. Implementing measures to support gut health, such as a balanced diet and stress management, can positively impact brain function and overall wellness. It is essential to prioritize gut health to maximize overall well-being and unlock our full potential.
Five Facts About The Gut-Brain Connection: Understanding Its Role in Health and Wellness:
- Your brain and gut are connected through the gut-brain axis.
- The vagus nerve plays a crucial role in the communication between your gut and brain.
- Neurotransmitters produced in the gut can affect emotions and feelings, such as serotonin and GABA.
- Gut microbes produce chemicals like short-chain fatty acids and bile acids, which can impact brain function.
- The gut-brain axis is connected to the immune system, and inflammation in the gut can lead to brain disorders.
FAQs about The Gut-Brain Connection: Understanding Its Role In Health And Wellness
What is the gut-brain connection?
The gut-brain connection refers to the communication system between the gut and the brain. These two organs are connected physically and biochemically, with the vagus nerve playing a significant role in transmitting signals in both directions.
How does the gut-brain connection affect emotions?
The gut-brain connection affects emotions through the production of neurotransmitters. Both the brain and gut cells produce neurotransmitters, such as serotonin and gamma-aminobutyric acid (GABA), that influence feelings of happiness, fear, and anxiety. Imbalances in these neurotransmitters can impact emotions and mental health.
Can gut microbes affect brain health?
Yes, gut microbes can influence brain health. They produce various chemicals, including short-chain fatty acids (SCFA), which affect brain function. SCFA can reduce appetite and influence reward-related brain activity. Gut microbes also metabolize bile acids and amino acids to produce chemicals that can impact the brain.
What role does inflammation play in the gut-brain connection?
Inflammation, often caused by an overactive immune system, plays a role in the gut-brain connection. Too much inflammation can lead to brain disorders like depression and Alzheimer’s disease. Inflammatory toxins, such as lipopolysaccharide (LPS), can pass from the gut into the blood, contributing to brain disorders.
How can probiotics and prebiotics improve gut-brain health?
Probiotics, also known as psychobiotics, are live bacteria that can positively affect brain health when consumed. They have been shown to reduce symptoms of stress, anxiety, and depression. Prebiotics, which are fibers fermented by gut bacteria, can also improve gut-brain health by reducing stress hormone levels and supporting a healthy gut microbiome.
What are some foods that support the gut-brain connection?
Omega-3 fats found in oily fish and fermented foods like yogurt, kefir, sauerkraut, and cheese are beneficial for the gut-brain connection. Omega-3s can increase good bacteria in the gut and reduce the risk of brain disorders. Fermented foods contain healthy microbes that can alter brain activity and support a healthy gut microbiome.